Morbidity and Mortality Associated with Dysnatremia in Patients with Severe Traumatic Brain Injury
Keywords:
Traumatic brain injury, head trauma, Dysnatremia, SodiumAbstract
Background:
Blood-brain barrier disruption is cited in the literature on severe Traumatic Brain Injury (TBI), manifesting as dysnatremia in some cases. The effect of the dysnatremia and clinical outcomes of TBI is not well studied. The present study aimed to evaluate the relationship between dysnatremia at admission time and outcome in patients with severe TBI.
Methods:
This was a retrospective study conducted on all adult patients admitted with severe TBI (Glasgow Coma Scale [GCS] <=8) in Peymanieh hospital of Jahrom city, south of Iran in 2017-2020. Dysnatremia In hospital mortality was the primary outcome; Vegetative state, severe disability, moderate disability, and good recovery were secondary evaluated outcomes. Demographic variables, vital signs, and trauma mechanism were also recorded. Univariate analyses for factors associated with mortality were performed.
Result:
A total number of 99 patients fulfilled the criteria for inclusion. Ten patients (10.10%) experienced dysnatremia. There was a significant relationship between dysnatremia and the outcome of treatment (X2 (8) = 40.81, P = 0.001) based on the cross-tabulation. There were significantly higher odds of death in patients with dysnatremia, compared to participants with normal sodium levels (OR=43.5, CI95%: 6.69 to 282.59). Getting a good recovery of disease had 0.101 (CI95%: 0.023 to 0.43) times lower odds in dysnatremic participants compared to participants with normal sodium levels. Other outcomes were not statistically different among study groups (P>0.05).
Conclusion:
Dysnatremia in the first 24 hours after traumatic brain injury could worsen the outcome.
Declarations:
Funding:
Jahrom University of Medical Sciences.
Authors' contributions:
ER, ME, and HA registered the study protocol. ME, NK, MR collected datasets. NK performed statistical analyses. All authors contributed to writing and editing the manuscript.
Acknowledgments
None.
Ethical considerations
The study was approved by the Institutional Review Board of Jahrom University of Medical Sciences with the code IR.JUMS.REC.1396.302.
UiEM promotes transparency in Peer-Review to achieve high-quality science. Where reviewers have not given permission of publishing review detail and their identity, the review process is visualized by Microsoft Word version track
changes algorithms. The peer-Review Track change of this manuscript is available by logical request via email.
---------------------------------------------------------------------------------------------------------------------
Full Text
Introduction
Increasingly studies have shown that Traumatic Brain Injury (TBI) can lead to electrolyte imbalance. Of all serum electrolytes, the most common electrolyte subject to imbalance in TBI patients is serum sodium (1). The severity of the head injury is a risk factor for the development of electrolyte disturbance in TBI patients. Dysnatremia as hyper or hyponatremia affects outcomes in TBI patients. Hypernatremia has been shown to increase mortality in critically ill patients, independent of comorbidities (1,2). The patients with hyponatremia resulted in a bad clinical outcome and a long stay in the hospital. They also have deterioration in clinical condition (3,4).
Patients with TBI have hyper and hyponatremia due to management during the hospital course. Induced hypernatremia is used to reduce acute elevations in ICP after TBI frequently (5,6). The previous study found that for the management of TBI, a number of therapeutic interventions can result in hyponatremia (7,8) disruption of the blood-brain barrier due to Traumatic Brain Injury (TBI) or a myriad of iatrogenic causes can lead to electrolyte imbalance. Although many studies have endorsed the effects of dysnatremia on the outcome of severe TBI patients, there is no study to differentiate the effect of iatrogenic and brain itself dysnatremia. The present study aimed to evaluate the relationship between dysnatremia at admission time and outcome in patients with severe TBI.
Methods
This retrospective study included all adult patients (age >=18 years) admitted with severe TBI (defined as a Glasgow Coma Scale [GCS] <=8) between May 2018 and April 2020.
The study setting was a university-affiliated teaching hospital (Peymanieh hospital) with an annual census of about 2000 patients.
TBI included two types isolated TBI and multiple trauma TBI. Isolated TBI included only traumatic brain injury. Multiple injuries included fractures at other sites or mild abdominal injury, pleural effusion, and lung contusion. Inclusion criteria were isolated severe TBI(GCS<=8), who did not have any of these exclusion criteria (i) admitted to hospital less than 24 h; (ii) renal insufficiency history (iii) use of diuretics, corticosteroids (iv) diabetes mellitus, pituitary tumor; craniopharyngioma(v) hemodynamic unstable(vi) lost to follow-up (vii). The participants were recruited from the electronic hospital information system by reviewing the admission records of patients. The following data were then collected for each patient from hospital records: demographic and injury data including age, sex, time from injury to arrival to the trauma center, mechanism of injury; clinical variables including GCS, blood pressure, heart rate, temperature, O2 saturation, and respiratory rate at admission, Laboratory data including serum glucose, hemoglobin, leukocyte and platelet counts, renal function, and serum sodium and potassium. As per hospital protocol obtained for each patient on arrival time when the intravenous line was inserted (1).
Hyponatremia was defined as serum sodium equal to or less than 130mEq/Hyponatremia was classified into 3 degrees of severity: mild hyponatremia(125mmol/L -130 mmol/L);moderate hyponatremia(120mmol/L-125mmol/L);severe hyponatremia(115mmol/L-120mmol/L);very severe hyponatremia(less than 115mmol/L).(9) serum sodium of 131 to 145mEq/dL was classified as the normal range and serum sodium of 146mEq/L or greater as hypernatremia (6). Hypernatremia was classified into 3 degrees of severity: mild hypernatremia (150 mmol/L Na < 155 mmol/L), moderate hypernatremia (155 mmol/L Na < 160 mmol/L) and severe hypernatremia (Na 160 mmol/L) (5). Two outcomes have been measured for all included patients; mortality as a primary outcome, and vegetative state, severe disability, moderate disability, and good recovery as a secondary outcome.
Univariate analyses for factors associated with mortality were performed using the chi-square test for categorical variables, and Fisher’s exact test for categorical variables was performed to compare the demographic data, hospital characteristics, and comorbidities in patients with and without hypernatremia and hyponatremia. (1,2) Statistical software (SPSS version 20.0) was used for statistical analysis. Crude Odds ratios (OR) were calculated based on the fisher exact test and expressed by OR and 95% confidence intervals.
Results
In the period June 2017 to September 2018, we enrolled 100 patients with STBI, One person was excluded from the study because of incomplete records. 99 patients fulfilled the criteria that were selected. The included patients were divided into 2 groups according to their serum sodium levels; one group with normal sodium level and another group with dysnatremia (hypernatremia or hyponatremia).89 patients had normal serum sodium (Na 135-145 mmol/L), 10patients had dysnatremia. Baseline demographic and injury data for the study set are shown in Table 1. Clinical data of patients including blood pressure, heart rate, respiratory rate per minute, body temperature, oxygen saturation was recorded. These results are shown in Table 2. No significant difference in clinical data was observed among the two groups. Paraclinical data including potassium, glucose, calcium, Pco2, creatinine and the bun level was recorded. These results are shown in Table 1.
Table 1. Baseline demographic and trauma mechanism and paraclinical disturbance
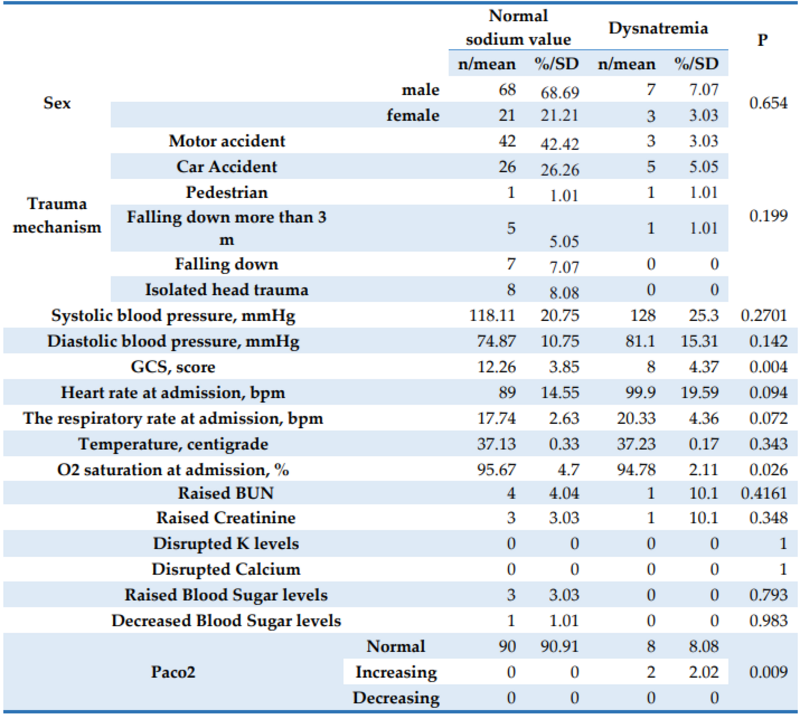
Table 2. Dysnatremia and outcome

Finally, to determine the association of TBI patient serum sodium variables on mortality Chi-square test was used. The overall results showed that there is a significant relationship between serum sodium values and the outcome of treatment (X2 (8) = 40.81, P = 0.001). There were significantly higher odds of death in patients with dysnatremia, compared to participants with normal sodium levels (OR=43.5, CI95%: 6.69 to 282.59). Getting a good recovery of disease had 0.101 (CI95%: 0.023 to 0.43) times lower odds in dysnatremic participants compared to participants with normal sodium levels. Other outcomes were not statistically different among study groups (P>0.05).
A number of 74 patients had a complete recovery that is one of them, serum sodium was high in the category of moderate hypernatremia, and the chi-square post hoc test showed a significant relationship (P = 0.001).
Discussion
To our knowledge, it is the first that has been aimed at investigating the incidence of dysnatremia on admission time in patients with severe TBI. The study shows that, in the immediate post-TBI period, during the 0- 3 hours after TBI, dysnatremia is associated with an increased risk of death and disability.
In our study dysnatremia was noted in 10 % of patients, with the majority of the patients exhibiting mild and moderate dysnatremia. However, in other studies, the incidence of dysnatremia is different and the rate of hypernatremia and hyponatremia is much more than in our study. In the study of Vedantam et al, hypernatremia was detected in 36.9% of patients. This study has the highest prevalence. (1) Also, the study of N.Moro et al hyponatremia had an incidence of about 33.0%. (7) This difference may be due to management during admission.
This incidence in Li et al article was 28%(6). In another study, Maria Tudor et al, the incidence of hyponatremia with TBI was 20 %. ( 8) In all of these studies, hypernatremia and hyponatremia have been calculated during admission time and are the important reason for the difference between the incidence of dysnatremia in The present study that evaluated the relationship between dysnatremia only at admission time and outcome after severe TBI. In the present study, we found a significant relationship between good recovery and normal sodium value. We had 75 patients with good outcomes only 4% of them had dysnatremia at admission time. The study by Li et al. had shown from 163 patients with good recovery only 9.2% of patients had hypernatremia.
The relationship between dysnatremia and disability has been documented in this study. In the moderate disability group, 10.0% of the patients had dysnatremia. it was as same as the vegetative state group and there were any patients in the group with mild disabilities with dysnatremia. according to the study of M.Li et al,7.7% of the patients with moderate disability and 54.2% with a severe disability had dysnatremia as hypernatremia. In this study also 58.4 % of patients with a persistent vegetative state had hypernatremia.
Limitations:
Our study had several limitations one limitation of this study was we did not perform a regression analysis to evaluate the role of different levels of sodium value in predicting outcomes. The study was conducted at a single center.
Conclusion
Dysnatremia in the first 24 hours after traumatic brain injury could worsen the outcome.
References
1. Aditya Vedantam, Claudia S. Robertson, and Shankar P. Gopinath. Morbidity and mortality associated with hypernatremia in patients with severe traumatic brain injury. Neurosurgery Focus 2017;43.
2. Haydn Hoffman, Muhammad S. Jalal, Lawrence S. Chin. Effect of Hypernatremia on Outcomes After severe Traumatic Brain Injury: A Nation-wide Inpatient Sample analysis. WORLD NEUROSURGERY 2018;1-7.
3. Ibrahim M. Alharfi, Tanya Charyk Stewart, Shawn H. Kelly, Gavin C. Morrison, Douglas D. Fraser. Hypernatremia Is Associated with Increased Risk of Mortality in Pediatric Severe Traumatic Brain Injury. JOURNAL OF NEUROTRAUMA 2013;361-366.
4. Umberto Maggiore, Edoardo Picetti, Elio Antonucci, Elisabetta Parenti, Giuseppe Regolisti et al. The relation between the incidence of hypernatremia and mortality in patients with severe traumatic brain injury. Critical Care 2009;13.
5. M. Lia, Y.H. Hu a, G. Chen. Hypernatremia severity and the risk of death after traumatic brain injury Injury.Int. J. Care Injured 2013; 1213–1218.
6. Pathomporn Pin-on, M.Med.Sc, Ananchanok Saringkarinkul, Yodying Punjasawadwong,
Srisuluck Kacha, Drusakorn Wilairat. Serum electrolyte imbalance and prognostic factors of postoperative death in adult traumatic brain injury patients. Medicine 2018;97:45.
7. Nobuhiro Moro, Yoichi Katayama, Takahiro Igarashi, Tatsuro Mori, Tatsuro Kawamata, Jun Kojima. Hyponatremia in patients with traumatic brain injury: incidence, mechanism, and response to sodium supplementation or retention therapy with hydrocortisone. Surgical Neurology 2007; 387– 393.
8. Roxana Maria Tudor, Christopher J. Thompson. Posterior pituitary dysfunction following traumatic brain injury: a review. Pituitary 2018.
9. K.L.L. Moving, H.G.M. Leufkens, A.W. Lenderink, A.C.G. Egberts. The validity of hospital discharge International Classification of Diseases (ICD) codes for identifying patients with hyponatremia. Journal of Clinical Epidemiology 2003;68:530–535.
Downloads
Additional Files
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Updates in Emergency Medicine

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.